How to Manage Gestational Diabetes
On you prenatal visit, your doctor break the news to you that you have Gestational Diabetes. Now what? You don’t know what to do or where to begin, and you have been feeling anxious and sleepless for the past few days. Gestational diabetes or GDM can be totally scary and unexpected, especially because you know have you worry about you and the baby growing inside your tummy.
But there’s good news! GDM can be managed in non-invasive, even natural ways. Even more, the condition can be reversed to a significant often without medication.
First, let’s take a closer look at GDM.
What is Gestational Diabetes?
This type of diabetes can occur even if you do not have a previous problem with your blood sugar or have not been diagnosed with any form of diabetes. Presently, it affects 2-10% (that’s roughly 135,000 to 200,000 women in the United States) of all pregnant women annually, typically developing around the 24th to 28th week of pregnancy.
Basically, GDM happens when a woman’s body is not able to use or make the insulin it needs for the demands of pregnancy, which typically mean about three times much more than what the woman requires before conceiving.
Symptoms of GDM
Gestational diabetes will present with similar symptoms to the other forms of diabetes, including:
- Increased hunger
- Excessive thirst
- Frequent urination
- Fatigue
- Lightheadedness or dizziness
- Blurry vision
Before worrying that you have the condition, remember that due to hormones, most pregnant women naturally experience some these changes and discomforts of pregnancy, such as a big appetite and more frequent visits to the toilet. But if you have risk factors/issues or symptoms that seem out of the “normal,” talking to your doctor would be a good idea.
Causes & Risk Factors
To date, there is no known cause for GDM, but there are several risk factors associated with this type of diabetes, including:
- Family history– if someone in your family has diabetes, you may be at risk since your genes or DNA may predispose you the disease Do check your family history and take measures below to prevent the condition from occuring
- Age– pregnant women more than 25 years old are at higher risk for developing GDM
- Ethnicity– Native Americans, African Americans, Latinos, and Asians have a higher tendency to develop GDM than Caucasians
- Weight– women who are overweight before being pregnant, as well as those who gain excessive weight during pregnancy are at high risk
- Previous Incidence– if you have had GDM in one of your previous pregnancies, you are more likely to acquire it again, than someone who has not had the condition before
What can happen with GDM?
Increased rate of miscarriage or birth defects –GDM may affect your baby’s major organs or result in physical abnormalities that may be life-threatening
Overnutrition or excess growth for your baby– this increases the likelihood that you’ll undergo cesarean delivery since with vaginal or natural birth, a large baby will be traumatic to the fetus
“Fat baby” or “big body” syndrome- although the pregnant mother’s insulin does not cross the placenta, the extra sugar does giving the unborn baby high sugar levels. In effect, the fetus grows abnormally large with excessive body fat. This is medically known as ‘macrosomia.’ Children with this syndrome are at higher risk for childhood obesity, breathing problems, and type 2 diabetes.
Heightens the likelihood of stillbirths– this refers to the birth of an infant that has died in the mother’s womb after having survived at least the initial 28 weeks of pregnancy
Low blood sugar– also called ‘hypoglycemia’ which can manifest with symptoms of shakiness, sweating, blurred vision, hunger and dizziness
Getting Tested
Your doctor ordered an oral glucose tolerance test (OGTT) to check if you have GDM. You will be instructed to consume a sugary solution, then your blood sugar will be measured from your blood sample typically after 2 hours (or as ordered by the physician).
If it comes back positive, treatment should begin as soon as possible to prevent further harm or complications for you and your baby.
If you’re diagnosed with GDM, don’t get too stressed out. You simply need to work with your doctor or healthcare providers to manage your condition in the best possible way. Complying with the recommended treatment will ensure that your baby stays healthy and that your health will be kept optimal throughout the rest of your pregnancy.
The general guidelines for screening state that:
- If your OGTT result is normal in weeks 27 through 31 of your pregnancy, you don’t need more screening.
- If you experienced GDM during one of your previous pregnancies, the screening should be done earlier (as early as the 13th week).
- Other reasons for early screening include previous delivery of a large baby, obesity, sugar in the urine, and family history for diabetes.
Like all other forms of diabetes, the management for GDM will commonly include:
1. Special diet plans – below are guidelines for pregnant women with GDM from a nutritionists; but you need to consult with your physician and nutritionist to plan the best meals for your unique condition
- Maintain a healthy weight. Avoiding obesity (especially before getting pregnant) places a mom-to-be at less risk for GDM and other pregnancy-related complications.
- Generally, a pregnant woman with GDM needs to have a daily food intake with 35-38 kilocalories per kilogram of ideal body weight.
- Your ingested protein should be approximately 20% of your daily kilocalories.
- Your carbohydrate intake should be 50-55% of your daily kilocalories.
- Your fat intake should be lower than 30% of the total kilocalories per day.
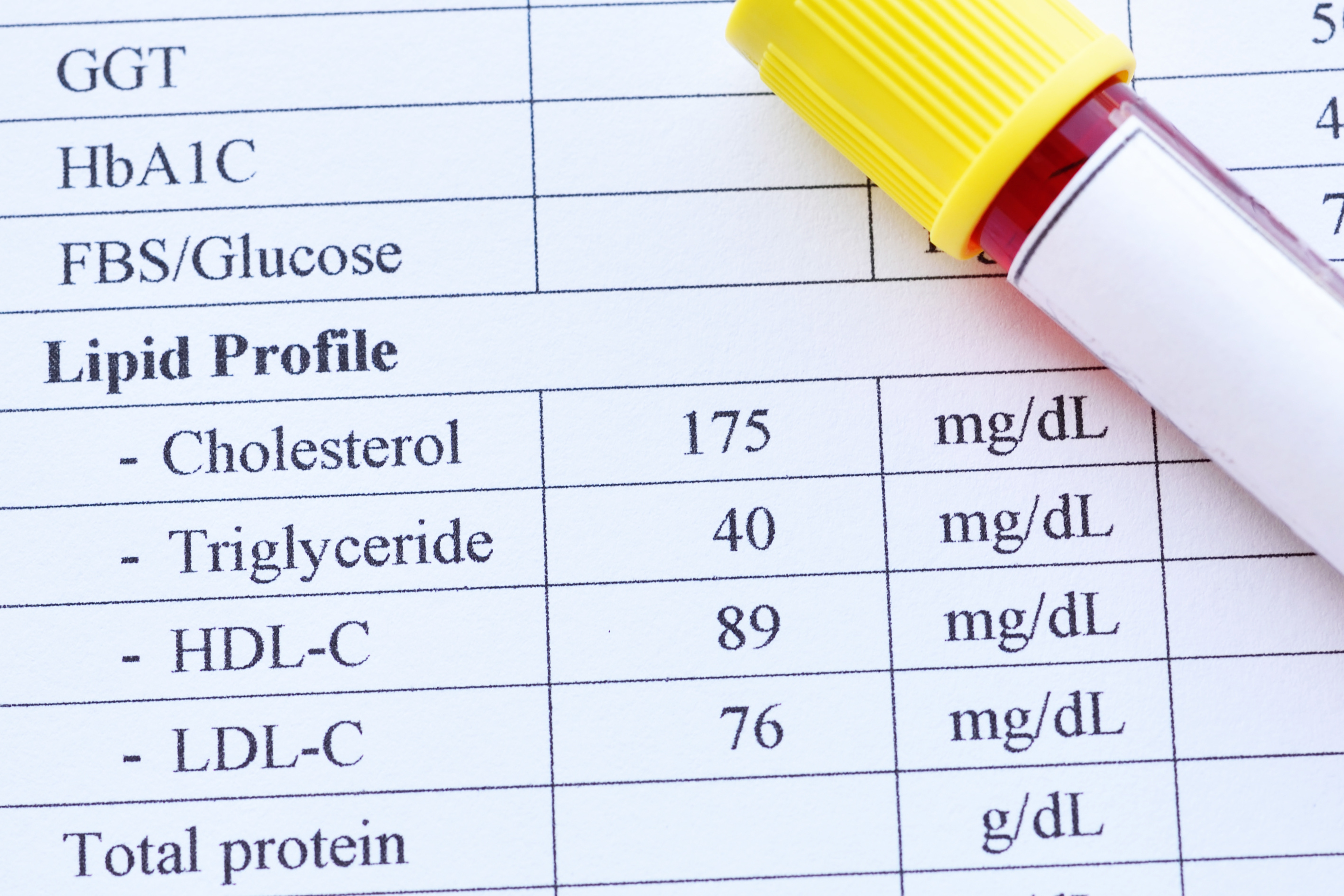
- Maintain a fasting and pre-meal sugar level below 90mg/dl.
2. Watching your weight- the appropriate weight gain should depend on your baseline body mass index (BMI) and weight before pregnancy. Talk to your doctor for ideal weight changes that should not go too low or too high
3. Scheduled physical activity– moderate exercise is beneficial in controlling your blood sugar levels and maintain a healthy weight during pregnancy
4. Daily blood sugar testing– women with GDM need to maintain stricter levels of blood sugar control during pregnancy; hence, blood sugar needs to be monitored more frequently (e.g., before meals, bedtime, occasionally an hour after eating)
5. Taking multivitamin supplements
According to a study of the Centers for Disease Control and Prevention (CDC), women who take multivitamins such as folic acid and B vitamins, significantly reduce the risk of birth defects for the baby.
Consult with your physician for the recommended multivitamin and mineral preparation for you.
6. Medications
- This commonly includes insulin injections to keep blood sugar within the controlled range throughout the pregnancy.
- Insulin is widely administered (as prescribed by the physician) if a pregnant woman’s diet does not sustain the fasting blood sugar (FBS) below 90 mg/dl.
- Insulin will typically be stopped at the time of the baby’s delivery (or as per advice of your physician).
7. Testing for defects
- Blood tests may be recommended by your doctor commonly at 15 weeks gestation to check for defects of the unborn baby.
- An ultrasound may be ordered at 18 weeks that can determine malformations for the growing fetus. This will not harm or be painful for the fetus or the pregnant woman.
- Some doctors request for a non-stress test, where a device will be placed on the woman’s abdomen to listen to the heartbeat of the fetus. When there is fetal movement, the heart rate of the baby normally speeds up by 15-20 beats per minute (this ‘speeding up’ should occur at least three times in 20 minutes)
Usually, GDM goes away after the birth of the baby. However, there are cases when women with the condition discover that they have diabetes (either type 1 or 2) that is no longer pregnancy-linked since signs and symptoms continue to show even after pregnancy. Statistics show that many women with GDM develop diabetes type 2 in the future. This is why a healthy, active lifestyle is recommended before, during, and after pregnancy.








 10 Low Sugar Snacks
10 Low Sugar Snacks